This activity is provided by Med Learning Group.
This activity is provided by Med Learning Group.
This activity is supported by an educational grant from Otsuka America Pharmaceutical, Inc. and Lundbeck.
Copyright © 2025 Med Learning Group. Built by Divigner. All Rights Reserved.

Diagnosing Agitation in Alzheimer’s Disease
The differential diagnosis in a patient with agitation and Alzheimer’s disease includes infection, dehydration, pain, and certain medications (eg, antihistamines, anticholinergics, opioids, corticosteroids, and sedatives). In addition to recognizing the pathophysiologic basis of agitation in Alzheimer’s disease, it is important to consider potential environmental factors, including a lack of predictable routines, overstimulation, understimulation, cognitive changes, emotional changes, and existing mood disorders.1,2
An actionable framework for symptom assessment and management is the “DICE” algorithm (ie, Describe, Investigate, Create, Evaluate). It begins with a description of the behavior from the caregiver in the context of a social and physical environment. Then comes an investigation of potential contributors to the behavior, including medication-related adverse events, pain, functional limitations, comorbidities, poor sleep hygiene, and sensory changes. Next is the creation of a multidisciplinary plan to address the agitation, which may include caregiver education, enhanced communication with the patient, meaningful activities to occupy the patient, simplifying complex everyday tasks, ensuring environmental safety, and adjusting the level of patient stimulation. Finally, the provider must regularly evaluate the efficacy of the approaches and consider if medication is warranted.2
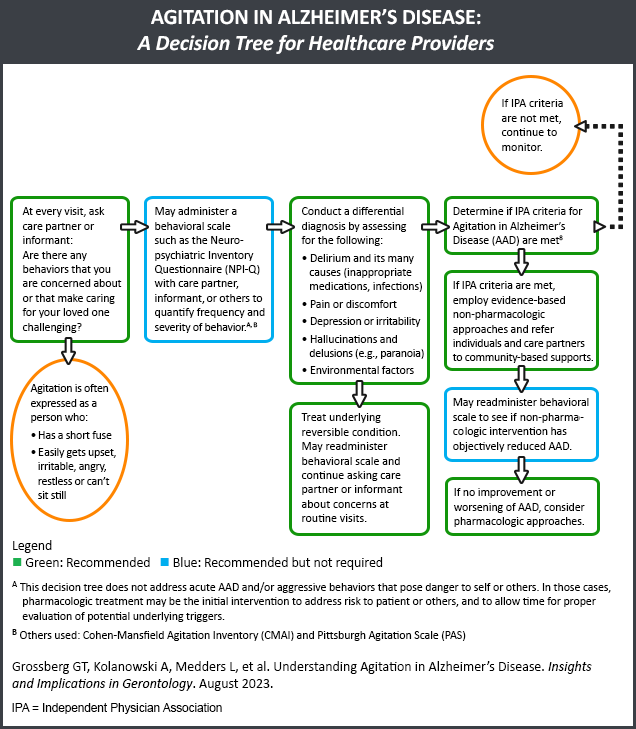
Agitation Decision Tree3
The Gerontological Society of America convened a group of experts to develop a decision tree to help healthcare providers diagnose and manage agitation in Alzheimer’s disease.3
Additional scales to assess agitation related to Alzheimer’s disease include the Behavior Rating Scale for Dementia, the Brief Psychiatric Rating Scale, the Psychogeriatric Dependency Rating Scale, the Multidimensional Observation Scale for Elderly Subjects, and the Revised Memory and Behavior Problems Checklist.4
The most commonly used scale, the Neuropsychiatric Inventory (NPI), measures multiple behaviors as assessed by a close family member.4 These include delusions, hallucinations, dysphoria, anxiety, agitation/aggression, euphoria, disinhibition, irritability, lability, apathy, and aberrant motor activity. Importantly, the NPI differentiates between disease severity and agitation frequency, while minimizing the time required for symptomatic assessment.5
References
- Koenig AM, Arnold SE, Streim JE. Agitation and irritability in Alzheimer’s disease: Evidenced-based treatments and the black-box warning. Curr Psychiatry Rep. 2016;18:3.
- Kales HC, Gitlin LN, Lyketsos CG; Detroit Expert Panel on Assessment and Management of Neuropsychiatric Symptoms of Dementia. Management of neuropsychiatric symptoms of dementia in clinical settings: Recommendations from a multidisciplinary expert panel. J Am Geriatr Soc. 2014;62:762-769.
- Grossberg G, Sanford A, Scanland S, Tracy K, Stefanacci RG. Agitation in Alzheimer’s disease: A decision tree for healthcare providers. Innov Aging. 2022;6(suppl 1):528.
- Geda YE, Schneider LS, Gitlin LN, et al. Neuropsychiatric symptoms in Alzheimer’s disease: Past progress and anticipation of the future. Alzheimers Dement. 2013;9:602-608.
- Cummings J. The Neuropsychiatric Inventory: Development and applications. J Geriatr Psychiatry Neurol. 2020;33:73-84.